Tiny pollution particles can cause major health problems. Our research shows how to minimize your risk.
Over the course of our lives, the quality of the air we breathe has a powerful impact on our health. Exposure to air pollution is linked to a higher risk of health challenges, including:
and even premature death. Particulate air pollution cuts the average person’s life short by nearly 2 years, according to the Energy Policy Institute at the University of Chicago.
Dirty air affects us all. The World Health Organization recently found that 99% of the world’s population breathes air with unhealthy levels of pollutants that include fine particulate matter from fossil fuel burning, wildfire smoke and other sources.
But there’s good news, too: Simple solutions to improve indoor air quality—especially portable high-efficiency particulate air (HEPA) cleaners—could lower our health risks and even cut transmission of infectious diseases such as COVID-19.
Scroll to learn more about how air quality impacts our health from infancy through old age—and how researchers in the UW Department of Environmental & Occupational Health Sciences (DEOHS) and our partners are testing new solutions, with a focus on the most vulnerable: children, essential workers, low-income communities and the elderly.
Protecting little lungs
Exposures in early life can influence health for a lifetime
Tracking wildfire smoke’s impact on pregnant people and kids to protect them both
During a massive wildfire event in 2014, DEOHS Affiliate Assistant Professor Elizabeth (Gribble) Walker sheltered at her home in Washington’s Methow Valley for 10 days without power or water with her two children, one a newborn.
 Walker and her two young children weathered a major wildfire in 2014, an experience that inspired her to lead Clean Air Methow. Photo: Courtesy of Walker.
Walker and her two young children weathered a major wildfire in 2014, an experience that inspired her to lead Clean Air Methow. Photo: Courtesy of Walker.

In “this incredibly thick smoke, [I was] worrying about my brand-new baby; my daughter, still young; my own health; everyone else in the community.”
–Elizabeth Walker on the Carlton Complex fires of 2014
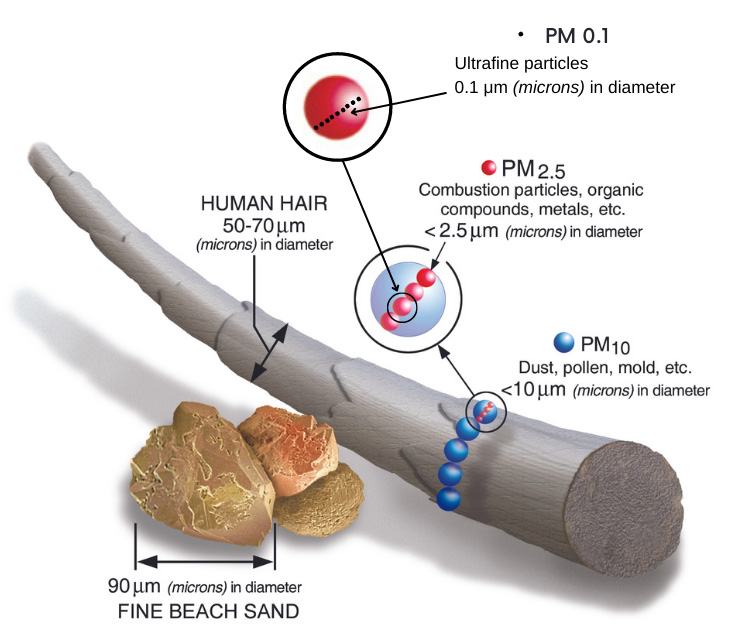
Wildfire smoke is made up of harmful components, including fine particulate matter (PM 2.5) that lodges deep in the lungs.
Infants and children are particularly sensitive to air pollution because of their small, developing bodies. Their exposure to PM 2.5 and other air pollutants is linked with reduced lung function, asthma and neurodevelopmental effects.
Some of those risks start before birth: Prenatal exposure is associated with a greater risk of infant mortality, preterm birth and low birth weight, and even the development of asthma and autism.

To learn more about impacts on the youngest in wildfire-prone communities, Dr. Catherine Karr, professor in DEOHS, and UW Senior Epidemiologist and DEOHS alumna Christine Loftus are partnering with researchers at Oregon State University to develop a study on pregnant people's exposure to wildfire smoke and the health impacts on their infants.
They are focusing on Klamath County, OR, which, like the Methow, has experienced frequent wildfires over the past decade, resulting in dozens of days of unhealthy levels of wildfire smoke per year.
Researchers will deploy indoor and outdoor air monitoring units and give silicone wristbands to volunteers to track their exposure to PM 2.5 and volatile organic compounds. The team will also survey health impacts on the parents and their infants once they are born.
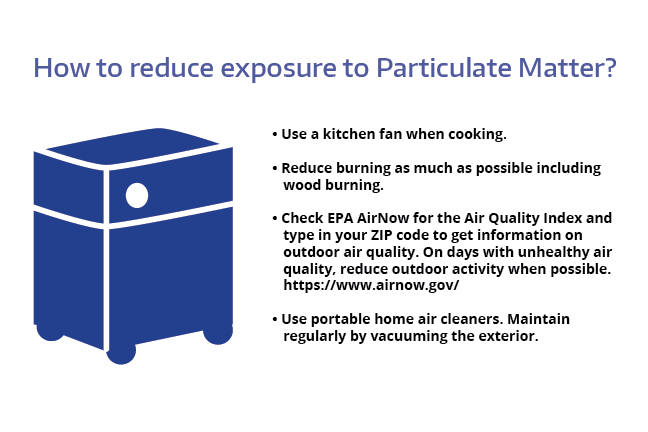
Walker, who now directs the community organization Clean Air Methow, emphasizes the benefits of cleaning air indoors, as that’s where people spend most of their time.
The group and their partners at the Okanogan River Airshed Partnership (ORAP) help residents in the region get “smoke ready.” That includes providing portable HEPA air cleaners and do-it-yourself box-fan filters to remove PM 2.5 and other pollutants.
“The vision? Clean indoor air for everyone. We need to start viewing air purifiers or filtration systems as standard safety equipment in the home.”
–Kris Ray, former ORAP director and air quality program manager for the Confederated Tribes of the Colville Reservation
Cleaner classroom air
Living near the airport is not just noisy—it can also make you sick
Partnering with airport communities to improve air quality for school kids
Ultrafine particulate matter (PM 0.1) from jet pollution pervades the air in communities around Seattle-Tacoma (SeaTac) International Airport, according to a 2019 study led by DEOHS Assistant Professor Elena Austin and colleagues.
When people inhale these invisible particles—about 700 times smaller than the diameter of a human hair—the particles can pass from the lungs into organs, including the brain. Ultrafine pollution particles are associated with negative effects on respiratory, cardiovascular and neurological health.
School-aged children could be especially vulnerable to some of these health impacts, and research suggests that air pollution can also influence brain development and academic performance.
“The question we got most often was, what could be done about it?” Austin said about her conversations with airport communities.
Austin and her colleagues deployed portable air monitors in classrooms to measure the particles and other pollutants and conducted tests with HEPA air cleaners in a project funded by the Washington State Legislature and five cities near the airport.
They found that using portable HEPA filter units could reduce classroom concentrations of ultrafine particles by about 70%.

“When many of the school districts we’re working with saw the results and heard concerns from parents, teachers and unions about air quality, they went ahead and used federal funds to purchase HEPA filters for their classrooms.”
-DEOHS Assistant Professor Elena Austin
Now researchers are applying the same approach to study schools in Central Washington that face wildfire smoke exposure. DEOHS PhD student Orly Stampfer is also developing a clean air curriculum for students in local schools.
Interactive graphic: See how you can improve indoor air quality
Simple steps can improve air quality in classrooms and other indoor spaces, including upgrading HVAC system filters to MERV-13 or higher efficiency; using a properly sized portable HEPA air cleaner; and, in some cases, opening windows.
Choose options below to see how interventions influence outdoor pollution sources such as traffic exhaust and indoor sources such as the novel coronavirus.
Indoor air quality concerns include COVID-19 and other airborne respiratory viruses (ultrafine particulates), as well as pollution from stoves (fine and ultrafine particulates), building materials (volatile organic compounds) and other sources.
Sources of outdoor pollution include exhaust from vehicles and aircraft, industrial emissions, wildfire smoke and other sources. They can comprise fine and ultrafine particulates, volatile organic compounds, gases such as nitrogen dioxide and other pollutants.
MERV-13 filters can remove more than 85% of fine particles and more than 50% of ultrafine particles. Installing them in a central HVAC system can remove varying amounts of indoor particulates depending on building conditions. Experts recommend setting systems at five air exchanges per hour.
Opening windows ventilates a room with outdoor air. This lowers the levels of airborne viruses such as COVID-19, but it is not recommended in areas with high levels of outdoor pollution or during wildfire smoke events.
Opening windows is not recommended in areas with high levels of outdoor pollution or during wildfire smoke events.
HEPA filters can theoretically remove at least 99% of ultrafine particles, and larger or smaller particles with even greater efficiency. In practice, using a portable HEPA air cleaner can remove up to 85% of indoor particle concentrations if correctly sized for the space with windows closed. Learn how to choose one for your needs.
Learn about interventions
Learn how these interventions affect different air quality concerns
These results are for illustrative purposes and results may vary in the real world. Sources: EPA; CDC Interactive Ventilation Tool; Healthy Air, Healthy Schools Project. Boxes represent approximate indoor or outdoor air composition; the illustrations of air pollution are not to scale.
Breathing easier on the farm
Farming communities struggle with many sources of air pollution, putting kids at risk
HEPA air cleaners help reduce asthma emergencies for children of farmworkers
In Washington's Yakima Valley, residents are breathing in numerous air pollutants from the region’s agricultural activity, including truck exhaust, fertilizers and pesticides, dust, wildfire smoke and gases such as ammonia released from animal waste on farms.
These contaminants irritate lungs and are suspected to contribute to the high rate of asthma problems among children of farmworkers in the valley.
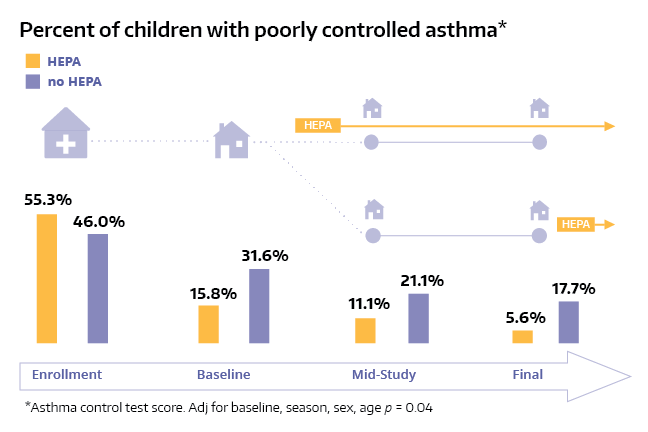
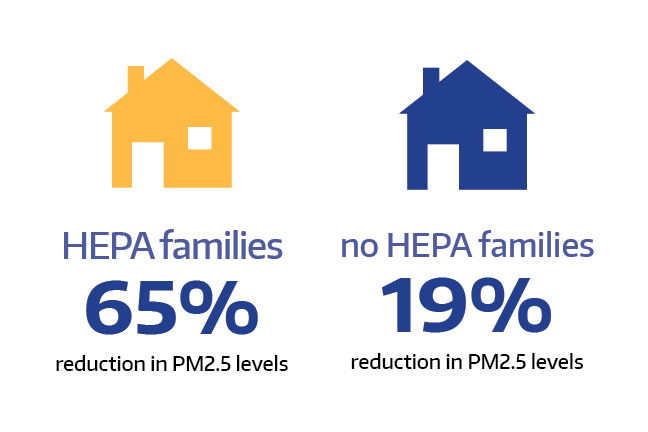
A DEOHS-led team tested a simple solution: putting HEPA air cleaners in the kids' bedrooms and living rooms.
Professor Catherine Karr and her team partnered with the Yakima Valley Farmworkers Clinic and community organization Northwest Communities Education Center/Radio KDNA (NCEC) to monitor environmental triggers for children with asthma.
"If we are serious about addressing health disparities in children, we need to address air quality disparities."
-DEOHS Professor Catherine Karr
Adriana Perez, community health services program manager for the clinic, coordinated the study, which included six home visits to 75 families over a year.
"The families would be happy to see us because they already knew us" through their connection to the clinic and NCEC, she said. "They had this trust in us."
Half the families were given asthma education and air cleaners, while the other half received education only. The education included green cleaning kits to reduce harmful chemicals in the air.
The children with asthma who used the air cleaners were 72% less likely to need unplanned medical care, the team found.
"One of the families in the lower Yakima Valley was so grateful," Perez said. "She noticed a huge improvement in her child's asthma and less emergency room visits as well."
At the end of the study, all the families were provided with air cleaners, and the clinic now recommends them to families who have kids with asthma. Because of the benefit and expense of these devices for families, Perez hopes air purifiers will eventually be covered by health insurance.
Partnering to ease kids’ asthma
Click on the images below to explore photos and conclusions from the study. Photos: Lisa Younglove. Graphics: Sarah Fish.





caption
Helping farmworkers through smoke season
Real-time data on air quality could help protect farmworkers and crops
Pairing new wildfire smoke sensors with Washington weather stations
Summer’s overlapping harvest and wildfire seasons in the Pacific Northwest pose an increasing health hazard for the region’s 140,000 agricultural workers.
For too many, there’s nowhere to go to escape wildfire smoke that permeates their homes and their outdoor workplaces in Washington’s fields and orchards.

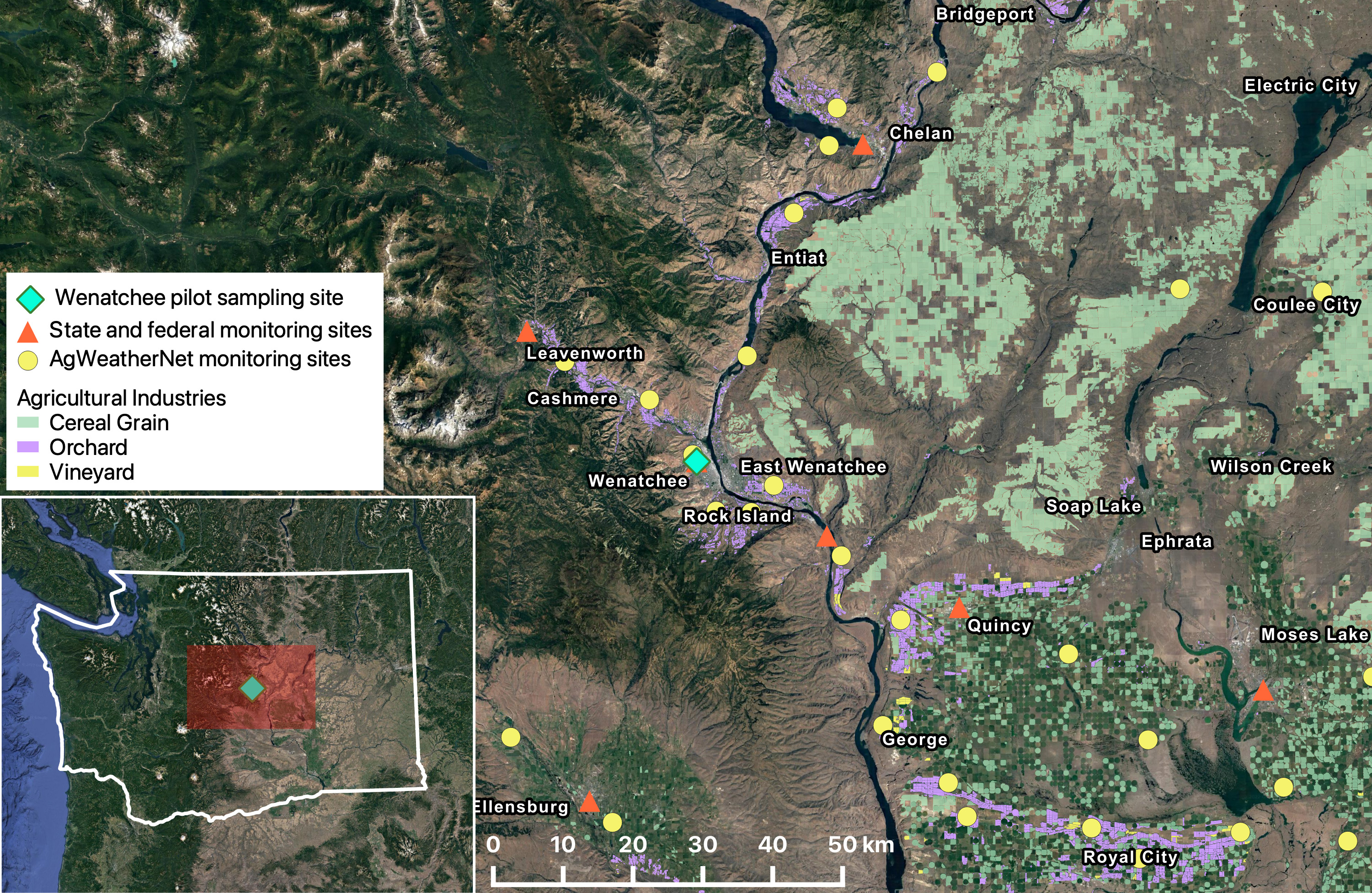
Better data on local air quality could help growers, managers and workers make better decisions about when, how and whether to work in smoky conditions. But regulatory air monitoring equipment is scarce in many rural areas, with only 35 state-run stations east of Washington’s Cascade Mountains covering a land area of 45,000 square miles (see map).
The Pacific Northwest Agricultural Safety and Health Center (PNASH), part of DEOHS, led a pilot project to evaluate two low-cost wildfire smoke sensors in 2020. The devices were placed alongside a state-run weather station in the agricultural hub of Wenatchee and performed as well as the state’s standard air monitoring equipment.
Now that project will expand to place 25 additional sensors at weather stations managed by Washington State University’s AgWeatherNet system, which is more widely distributed across Eastern Washington.
“Having real-time, highly localized data on air quality can lead to better decisions in the field about protecting worker health and safety as well as crops,” said DEOHS PhD student Claire Schollaert, who led the pilot project with Edward Kasner, DEOHS clinical assistant professor.
Ideally, farmers and growers will access the data directly through a public web portal. The information could also help agricultural employers meet new state health and safety standards likely to be created this year for wildfire smoke exposure in the workplace, Schollaert said.
The new phase of the project is funded by the Washington State Department of Labor & Industries in partnership with PNASH and the Washington State Tree Fruit Association.
Pandemic-proofing public spaces
Improving indoor air quality can limit COVID-19 transmission
Advising Washington businesses and schools on how to stem the pandemic
When the pandemic began, Martin Cohen began getting calls from local businesses and schools about how to safely reopen. Cohen, an industrial hygienist and teaching professor in DEOHS, directs the department’s Field Research and Consultation Group.
In response, Cohen formed the DEOHS Return-To-Work Task Force, drawing from the department’s cross-disciplinary experts to advise on workplace safety protocols for more than two dozen companies, including the Paramount Theatre, Sony Pictures, the Space Needle and the Seattle Aquarium.
"Typically, we've used what I tend to call the Swiss cheese approach—focusing on helping entities do many different things to make safe spaces, because not everything is going to be perfect," Cohen said.
The group’s advice includes recommending masking, increasing ventilation with outdoor air, increasing filtration of recirculated air in a central heating, ventilation and air conditioning (HVAC) system with MERV-13 or higher-efficiency filters, and decreasing the number of occupants in a space.
MERV-13 filters can remove more than 85% of PM 2.5 and more than 50% of ultrafine particles, including the novel coronavirus.
HEPA air cleaners, which can capture more than 99% of ultrafine particles, help reduce viral concentrations in the air if they're sized correctly for the space, Cohen said.
His advice for homeowners and business owners: If your space is relatively small and you're not able to provide more outdoor air or filter it better—for example, during a wildfire smoke event—get a portable HEPA air cleaner.
Air pollution could raise dementia risk
Our lifelong exposure to air pollution can take a serious mental toll
Using big data to tease out traffic pollution’s threat to brain health
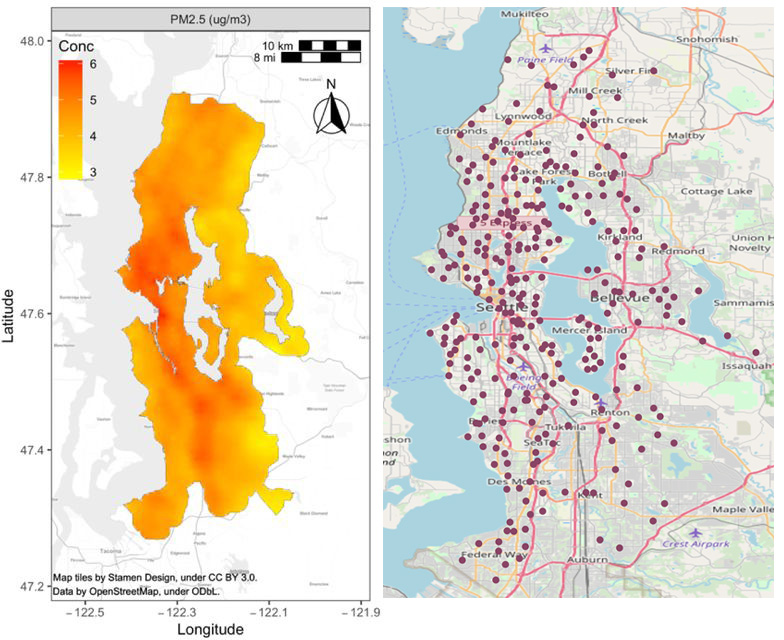
Puget Sound residents exposed to higher levels of fine particulate air pollution over a 10-year period had a greater risk of developing dementia, according to a recent study by DEOHS Professor Lianne Sheppard and colleagues.
“If you think about it on a population basis, and the fact that everybody is exposed to air pollution, … if this association is causal, it suggests that there are a lot of people who are going to be impacted,” said Sheppard.
Their results rely on a longitudinal study of 4,000 Seattle-area residents and local air pollution data collected by DEOHS Professor Timothy Larson and others that extends back to the 1970s.
“We want to encourage policy change to reduce exposure to the whole population,” said Rachel Shaffer, a DEOHS PhD alumna and first author of the study. “There’s not really a threshold of exposure that’s safe.”
In another recent study that Sheppard designed to monitor traffic-related pollution, DEOHS PhD alum Magali Blanco and collaborators drove around Seattle with car-mounted air sensors.
They measured pollutants including ultrafine particles, nitrogen dioxide, carbon monoxide and carbon dioxide in about 300 off-road locations.
They found that annual average ultrafine particle concentrations were highest downtown, near the airport and along highways.
Next, the team plans to examine how traffic-related air pollution exposures compare to the incidence of dementia in these areas.
“If we find any meaningful connections, that will contribute to the body of evidence that can be used to make policy changes to protect public health,” Sheppard said.
Ensuring health equity
Air pollution affects us all, but we are not all affected equally
People of color (%)
PM 2.5 concentration
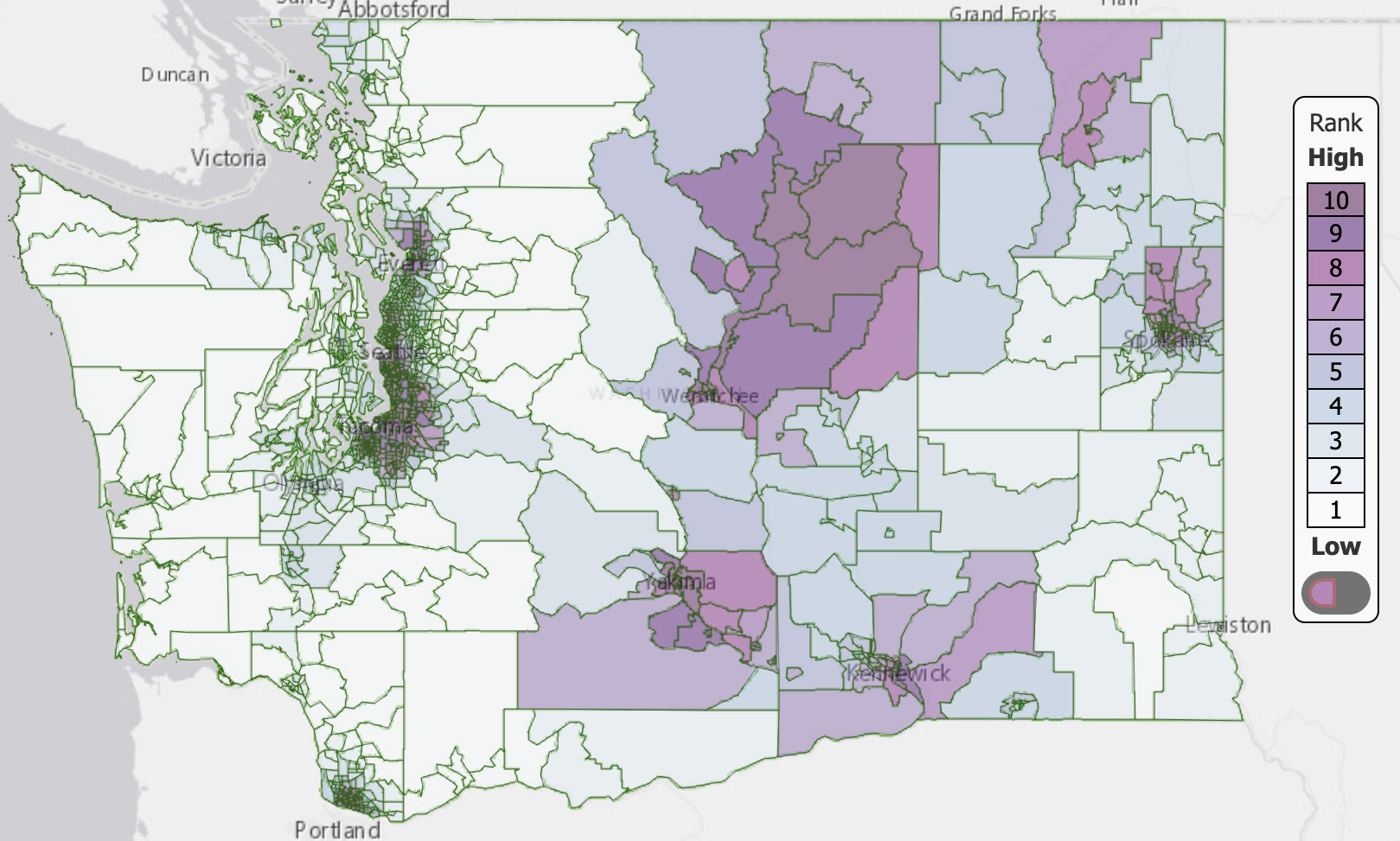
Mapping environmental health disparities and helping the most vulnerable
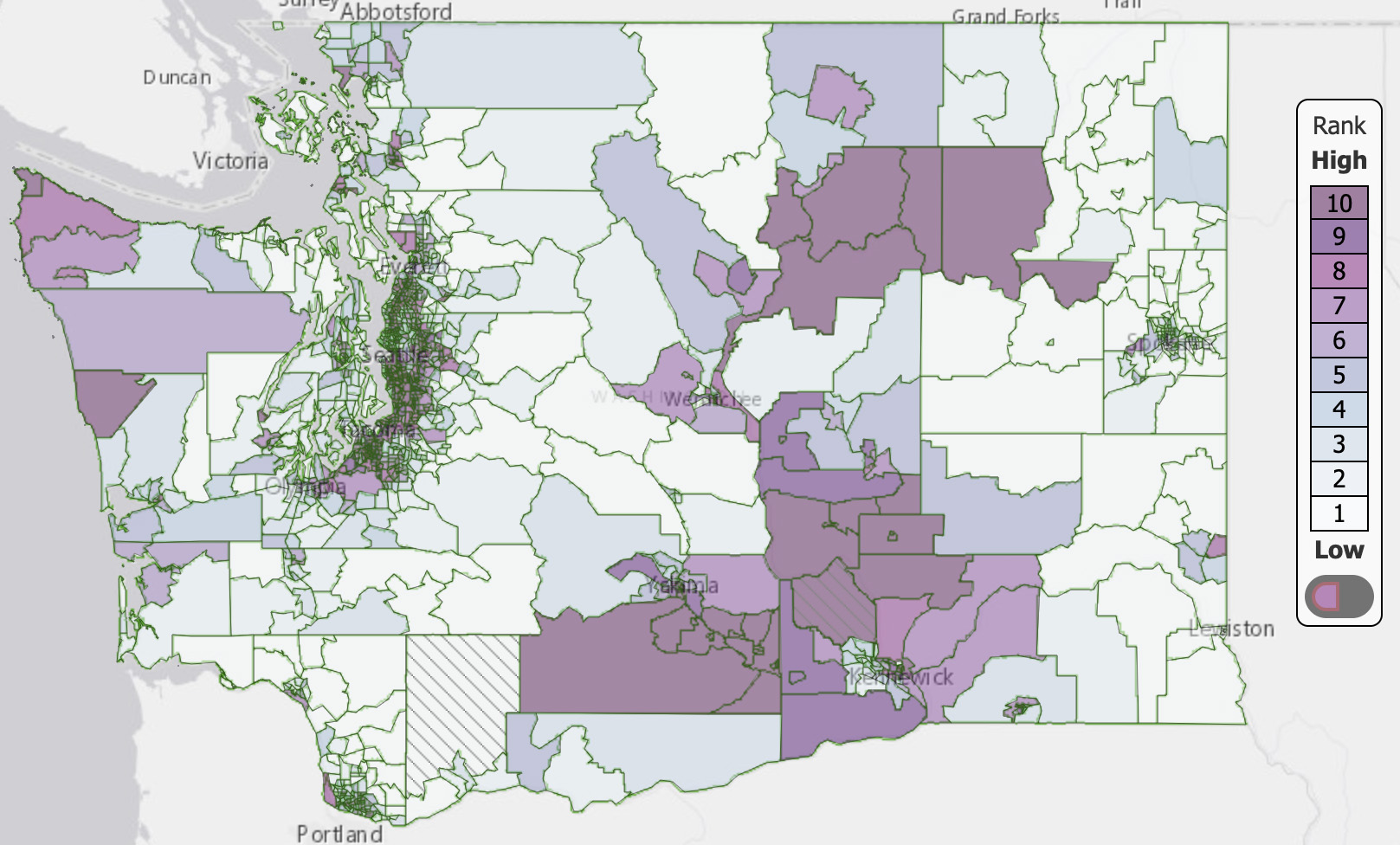
In Washington state, areas with high levels of air pollution—such as communities near highways and airports—tend to be home to a higher proportion of Black, Indigenous and people of color (BIPOC) and low-income residents than other parts of the state, DEOHS research shows.
These environmental health disparities are one of many legacies of the history of redlining and discrimination in Washington and across the US.
DEOHS Clinical Assistant Professor Esther Min, Associate Professor Edmund Seto and their colleagues created the Washington Environmental Health Disparities Map to provide a framework for understanding and comparing these disproportionate environmental impacts.
Now, DEOHS PhD student Nancy Carmona is developing a new air pollution risk layer for the map so that people can easily view how air pollution levels where they live relate to national air quality standards.
To help improve indoor air quality for some low-income residents in the state, Seto is partnering with Public Health — Seattle & King County to install and test the impact of HEPA air cleaners in homeless shelters around King County.

"By harnessing data to pinpoint environmental inequality, it’s possible to show precisely where the state’s most highly impacted communities are concentrated and create customized solutions to reduce their risk."
–DEOHS ASSOCIATE PROFESSOR EDMUND SETO
More resources
- Wildfire smoke and children's health: A new training module for nurses developed by MaryKate Cardon, co-director of the Pediatric Environmental Health Specialty Unit, part of DEOHS.
-
Air pollution and your health: Information from the National Institute of Environmental Health Sciences.
-
Improving indoor air quality: Information about pollution control, improved ventilation and air cleaners from the US Environmental Protection Agency (in English and Spanish).
-
Short EPA video on how to improve indoor air quality.
-
Fresh air for a healthier home: Information from the Washington State Department of Health.
-
3 ways to improve indoor air during the pandemic: Information from Public Health — Seattle & King County.
-
Resources on wildfire smoke safety: Information from the Pacific Northwest Agricultural Safety and Health Center, part of DEOHS.
-
Our air pollution research: Learn more about DEOHS’s work to promote clean air.
Published May 17th, 2022
This special feature produced by the DEOHS communications team: Veronica Brace, Jolayne Houtz, Deirdre Lockwood and Nick Nemetz. Editorial direction: Deirdre Lockwood; design and production: Veronica Brace. Images (top to bottom): Hollie Santos on unsplash, Courtesy of CDC on unsplash, Bonnie Kittle on unsplash, USDA on Flickr, airfocus on unsplash, Dario Valenzuela on unsplash, and Cheng Huang on unsplash.



