“How can we make our operating room safer during the pandemic?”
When Dr. James Hecker, an anesthesiologist at UW Medical Center, heard this question from a fellow physician, he thought about the problem not just as a doctor but also as an engineer.
Hecker, who has a PhD in chemical and biomedical engineering, knew about the risks of airborne transmission of the novel coronavirus. It can remain in the air for hours on microdroplets released after someone with the virus coughs, sneezes or talks. These aerosols can also be produced during medical procedures, raising concerns for both patients and health care workers.
But how such infectious aerosols might spread indoors—particularly in medical centers—is not well understood.
To learn more, Hecker and Igor Novosselov, research associate professor in Mechanical Engineering and adjunct research associate professor in the Department of Environmental & Occupational Health Sciences (DEOHS), launched a study to track the movement of aerosols in operating rooms using state-of-the-art sensors designed by Novosselov.
The project recently received $25,000 in funding through the new Director’s Award from UW CoMotion, a university hub supporting collaborative research. The team includes Edmund Seto, associate professor in DEOHS, Martin Cohen, DEOHS principal lecturer and assistant chair and many other UW physicians and researchers.
“I am trying to help to bring the incredible talent and technology at the UW into the sometimes insulated environments of our hospitals,” Hecker said.
Fishing for aerosols
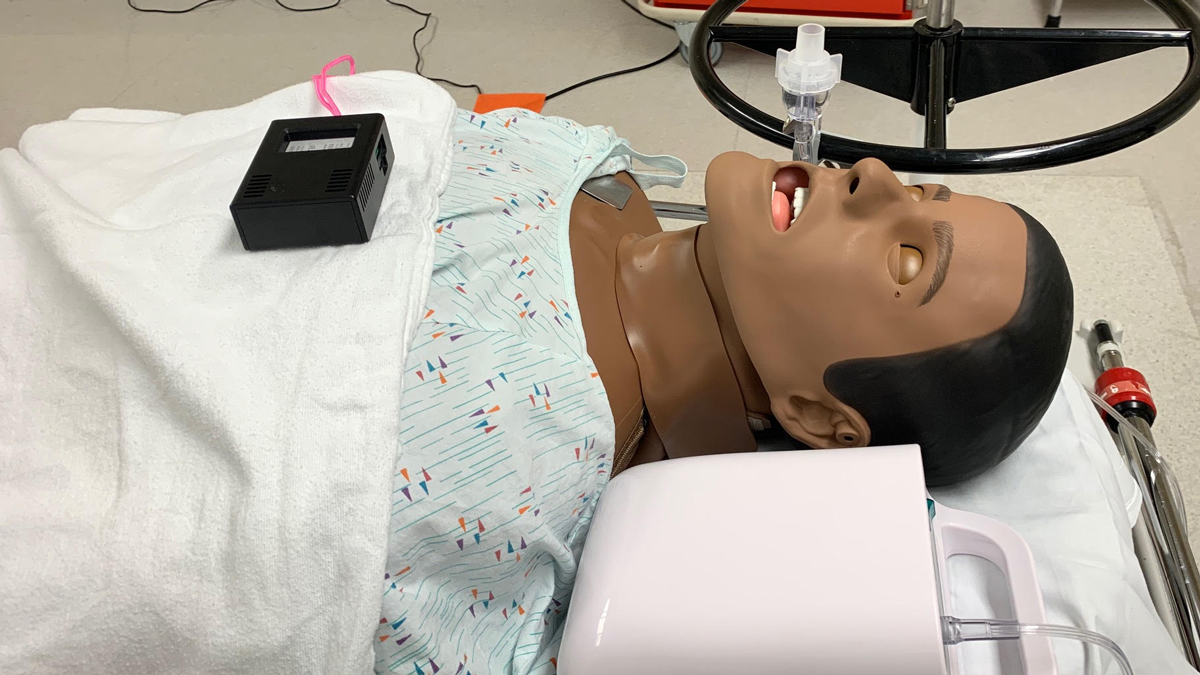
Last week, the team began its first on-site experiments in UW Medical Center’s WISH, a simulated operating room used for training. They outfitted the room with dozens of Novosselov’s air monitoring sensors, each about the size of a deck of cards.
Then the researchers used a medical nebulizer to create harmless saline particles that mimic aerosols and followed them to see where they went.
They are searching for spots where air currents might trap aerosols and keep them from being flushed out by the hospital’s ventilation system.
Novosselov likened these areas to a bend in a stream, where eddies form. “That’s where you want to go fishing,” he said.
The sensors report particle counts in real time, allowing the scientists to model the distribution of aerosols at different heights and locations in the room, and to see how they are affected by people moving through the space.
“We're trying to characterize the entire room,” Novosselov said.

Into the operating room and beyond

In the next few weeks, the team plans to set up a similar experiment in a vacant operating room at Harborview Medical Center with strict ventilation controls.
They will trace air currents with a fogging machine developed by Cohen, who directs the Field Research and Consultation Group, a DEOHS unit that provides occupational hygiene services to Washington businesses.
Cohen will also offer occupational hygiene guidance as the team contemplates potential solutions to these issues, including personal protective equipment and ventilation, such as vertical curtains of air around patients that would prevent aerosol dispersion.
The team’s findings could also inform practices in the emergency department, intensive care units and other parts of Harborview.
“It's important to protect everybody in the hospital—patients, doctors, nurses, the transporters, the pharmacists, the people that are delivering food, the people that are cleaning the operating rooms—everybody who has potential exposure,” Hecker said.
Eventually, the sensors could also be used as real-time monitors for indoor spaces, Novosselov said. The team is exploring commercializing the technology.
“If we can make it robust enough, it could be used not only in ICUs and emergency departments, but also in office-based anesthesia and non-health-care areas like gyms,” Hecker said.
Other researchers involved in the study include François Baneyx, vice provost for innovation, director of CoMotion and professor of chemical engineering; Dr. John Bramhall, associate professor of anesthesiology and associate medical director of Harborview Medical Center; Dr. Chris Barnes, ICU and general anesthesiologist; Dr. Arman Dagal, associate professor of anesthesiology and pain medicine, and director of spine and orthopedic anesthesia at Harborview; Dr. Joel Kaufman, professor of DEOHS, epidemiology and medicine; Amy Kim, assistant professor of civil and environmental engineering (CEE); Tim Larson, professor of CEE and DEOHS; Dr. Abhijit Lele, Neuro ICU director and neuroanesthesiologist at Harborview; Scott Meschke, DEOHS professor & assistant chair; Dr. Pratik Patel, ICU and neuroanesthesiologist at Harborview and Michael Yost, professor & chair, DEOHS.