Adding flame retardants to consumer products was supposed to protect people from harm when manufacturers began the practice in the 1970s.
Today, we are still learning about the long-lasting damage to human health and the environment caused by flame-retardant polybrominated diphenyl ethers (PBDEs) that were added to products ranging from furniture to children’s pajamas to car seats.
US companies stopped using most PBDEs by the early 2000s. Still, these hardy chemicals persist in our food chain, and epidemiologists have suggested there is a potential link between PBDE exposure and diabetes.
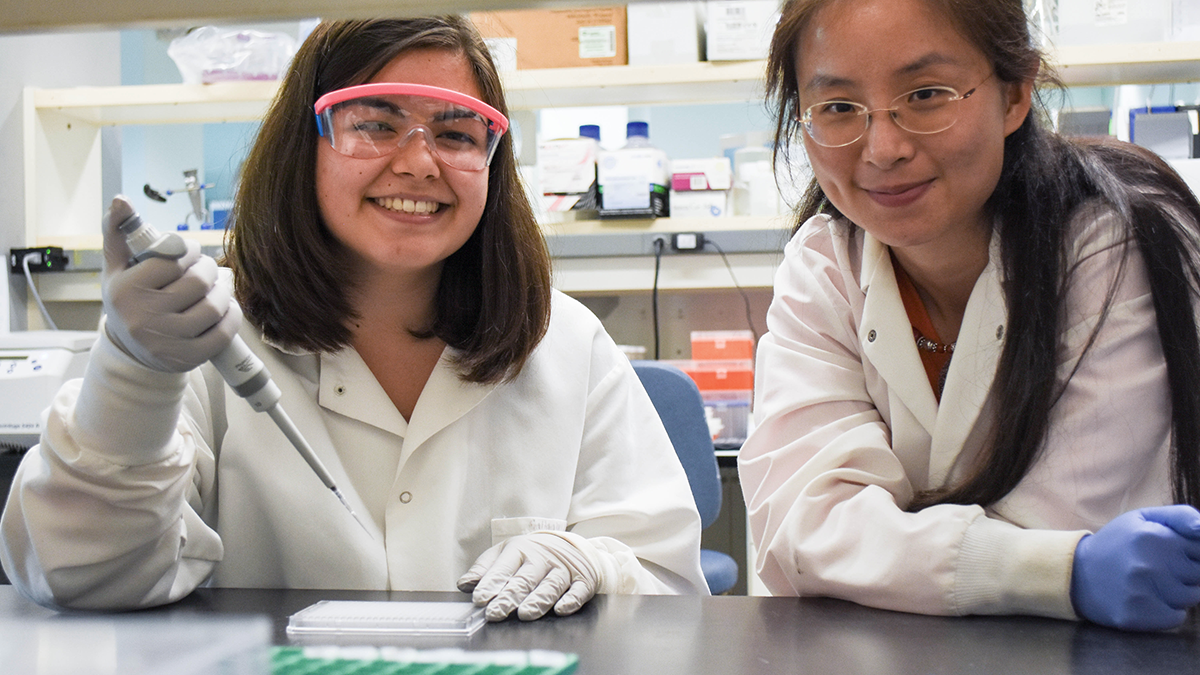
That link is the focus of new research led by Julia Yue Cui of the UW Department of Environmental & Occupational Health Sciences (DEOHS), supported by a five-year, $3 million grant from the National Institutes of Health.
Her team will conduct mouse experiments investigating how early-life exposure to PBDEs in breast milk may disrupt the normal activity of microbes in the gut, potentially boosting the risk of diabetes.
Insights from this research could aid future efforts to prevent diabetes in humans.
Going with the gut
The new project builds on years of work by Cui, DEOHS assistant professor, to illuminate the health effects of exposure to environmental contaminants, particularly in newborns.
Her team has explored how the gut microbiome interacts with host drug-processing genes in adult mice to modify the metabolism of PBDEs and how early-life exposure to chemical activators for host drug receptors alters drug-metabolizing enzymes in the mouse liver.
Last year, they reported that PBDE exposure in adult mice decreases amounts of substances produced by gut microbes that are known to protect against diabetes.
Now, in collaboration with researchers at Albert Einstein College of Medicine and Arizona State University, Cui and her team will test the long-term effects of early-life PBDE exposure-driven changes to the gut microbiome in adult mice.
“We hypothesize that PBDE exposure in infants might increase the risk of diabetes by reducing beneficial substances made by gut microbes and increasing harmful substances,” said Cui, who is the Sheldon D. Murphy Endowed Chair in Toxicology and Environmental Health.
The DEOHS microbiome initiative
Cui is part of a DEOHS research initiative launched in 2017 to study microbiomes at the human-environment interface, an emerging field of research that reflects a growing body of evidence that microbiomes are essential across diverse ecosystems.
All animals, including humans, are colonized by diverse microorganisms whose combined genetic capacity is a hundred-fold greater than our own, said DEOHS Professor Gerard Cangelosi, who leads the initiative.
“Microbial functions impact every step of human development, from birth to death,” he said. “Our microbiota play critical roles in how our bodies interact with our environments.”
“Our department is actively expanding our efforts in this area, and Dr. Cui is leading the way with her research,” Cangelosi said.
It’s an emerging and exciting field of scientific inquiry, said DEOHS Chair Michael Yost.
“Our department sees this as a prime opportunity for broad, cross-cutting research collaborations across the university, leading to interventions that could provide health benefits for individuals, communities and whole populations,” Yost said.
The mouse-human connection
For Cui’s current project, newborn mice will be exposed to PBDEs through placental transfer and breast milk from their mothers, who will receive PBDE-dosed food.
As with much of Cui’s research, a key component of this project is the use of mice that are genetically altered to be more similar to humans.
These mice have a gene for a protein called pregane X receptor (PXR), which is involved in diabetes in people.
The researchers will pay close attention to any diabetes-promoting changes to PXR that may be caused by PBDEs.
As the mice grow to adulthood, Cui and her team will monitor their microbiomes and analyze expression of mouse genes that are involved in diabetes.
“We hope to understand how PBDEs affect the gut microbiome to modulate the hepatic PXR signaling and diabetes-related processes during development,” said Cui. “Since mice and humans share many molecular processes, our work could provide strong clues about what happens in people.”
Working toward “living drugs”
“The holy grail would be to identify microbial species that could be given as ‘living drugs’ to people likely to have had high PBDE exposure while breastfeeding,” Cui said. “The microbes would produce beneficial metabolites that lower diabetes risk.”
Later stages of the new project will explore whether an increased risk of diabetes could be reversed by providing beneficial microbial products to mice exposed to PBDEs in breast milk.
Ultimately, collaboration with epidemiologists is needed for humans to benefit from mouse studies like these.
Cui has worked with Seattle Children’s to study how the human gut microbiome develops throughout childhood. “None of this work would be possible without my team of graduate and undergraduate students, my postdoctoral fellows, my research scientists and our collaborators,” she said.