As unprecedented as the outbreak of COVID-19 felt, it was far from the first time a deadly disease has swept the globe. Historians have identified epidemics and pandemics dating as far back as 430 B.C. Records tell us how these diseases spread and how many people died, but not people’s personal experiences of the crises.
COVID-19 presented a rare opportunity to document in real-time how people processed the tumult of a pandemic, and how necessary public health measures affected their lives. Starting in the earliest days of the 2020 outbreak, a team of researchers at the University of Washington conducted real-time surveys of King County residents, asking what measures people had taken to protect themselves, how their daily lives had been affected and what worried them most.
The results, published in February in the journal PLOS One, provide a glimpse into the subtle effects that public health measures like social distancing and stay-at-home orders had on the community.
UW News spoke with Kathleen Moloney, research scientist at the UW Collaborative on Extreme Event Resilience, and Nicole Errett, a UW assistant professor of environmental and occupational health sciences and director of the new Center for Disaster Resilient Communities, to discuss the study, how people experienced those early months and what public health practitioners can learn for future pandemics.
It’s been four years since COVID-19 changed all our lives, and more than two years since we started to emerge into this new normal. Why is it important to share this research now, to understand people’s experiences of the pandemic and collective efforts to limit COVID’s spread?
Kathleen Moloney: Unfortunately, COVID-19 is unlikely to be the last pandemic we face. To fully understand this pandemic’s impacts and better prepare for the next, we need research studies like ours — where data was collected in real time, from March to May of 2020 — that document the lived experiences of communities during the pandemic. For example, by documenting how people in King County experienced the social distancing measures in real-time, our study provides valuable insights into which negative impacts were most acute during the early stages of the pandemic. Our results, combined with evidence from other research studies, can provide direction for researchers and policymakers to explore effective interventions for future pandemics.

Nicole Errett: It is really important to start collecting data in the immediate aftermath of a disaster to understand effects on health and well-being, but researchers face a variety of administrative, logistical and ethical challenges when designing rapid-response research studies. By sharing our approach in this paper, we can provide ideas and guidance for other investigators while designing studies for future disasters, whether those are caused by an infectious disease or natural hazard.
You evaluated participants’ well-being as described in their written stories about their experience. What trends appeared there, and were they what you expected to find?
KM: Two findings surprised me in particular. First, less than half of our participants described impacts to their social life — I expected the percentage to be much higher. It would be interesting to know how that result might change if we surveyed the same participants at a later point in the pandemic, when social distancing measures had been in place for longer. I was also surprised to see the poorest average well-being reported by those over the age 65, and the highest average well-being reported by 18-to-34 year olds. This is in contrast to several other national-scale studies in the US and Europe, which found worse mental health impacts in young adults.
Given that older adults are more likely to reside alone in the U.S. than in most other countries and report high rates of social isolation and loneliness even during non-pandemic times, interventions to mitigate the mental health impacts of future pandemics on older adults probably deserve special attention.
In their written responses, participants most frequently described a negative financial or employment-related impact, even more than social impacts. How might that change how we prepare to help people through future crises?
KM: Knowing which negative impacts are most prevalent at various points in the pandemic, and how these impacts differ between groups, can help us develop more specific, more effective interventions to prevent these unintended consequences in the future. We saw that employment and financial impacts were the top concern for every age group except those 65 and older — this group expressed higher concern about physical health and social impacts. So while an early intervention to mitigate the financial impacts of a future crisis on younger adults could be effective, we would likely want to prioritize different resources for older adults.
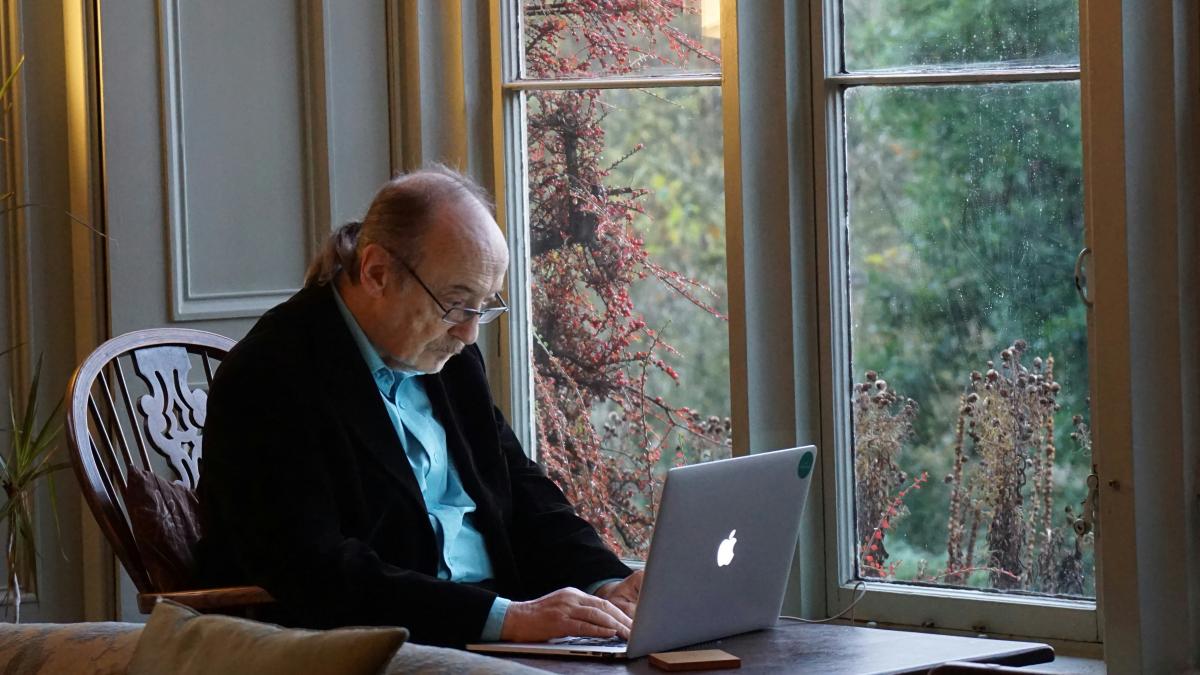
NE: The pandemic influenced the development — or at least accelerated the uptake — of systems that allowed many folks to work safely from the comfort of their own home without financial or employment impacts. However, folks with jobs in “essential” services and sectors often had to physically report to work, and often interface with the public. My colleague, Marissa Baker, found that folks that couldn’t work from home are lower paid. Accordingly, I’d suspect that employment and financial concerns would be disproportionately borne among lower wage workers, who would have to choose between their health and safety and their income. In advance of the next pandemic, we need to figure out ways to keep these folks safe and at work.
For more information, contact Errett at nerrett@uw.edu or Moloney at kmoloney@uw.edu.
Adapted from the original post here.