
“Get home safe” is one of the most commonly stated goals in worker health and safety. But what if you’re worried about bringing workplace exposures — viral, chemical or mental health-based — to those you live with?
About a decade ago, Diana Ceballos was evaluating health hazards for workers as an industrial hygienist with the National Institute for Occupational Safety and Health when she noticed a disturbing trend.
In many workplaces where lead contamination was an issue — including construction sites, battery and e-waste recycling plants, shooting ranges and auto shops — children of workers were experiencing lead poisoning.
“It shocked me to see that in this century,” said Ceballos, now an assistant professor in the UW Department of Environmental & Occupational Health Sciences (DEOHS). “Some of the workplaces were only put in the spotlight once the lead poisoning was happening [to kids], but not when they had a lead issue [in the workplace].”
The experience inspired her to focus on preventing such take-home exposures, in which workers inadvertently transmit chemical, biological or psychosocial hazards to their families or housemates.
The field has a history going back hundreds of years, including discoveries that the wives of coal miners were dying of black lung disease, and families of asbestos workers were contracting mesothelioma.

Now Ceballos and other researchers in DEOHS are engaging workers and their families in efforts to reduce take-home exposures in a wide range of professions, including healthcare, construction and agriculture.
While Ceballos is developing cutting-edge tools to identify and minimize these exposures, other DEOHS researchers are tracing the biomedical roots of the problem using novel biomarkers. What they share is an effort to give workers a voice in developing solutions.
“One of the things that goes very close to my heart is every time families are affected, they’re usually the low-power, no-health-insurance kind of families,” Ceballos said. “It’s very heartbreaking because they don’t have a voice.”
She explored these structural vulnerabilities in a review paper, noting that documented take-home exposures primarily affect racial or ethnic minority, young, low-income, temporary or immigrant workers and their families.
Leaving lead at work
Construction workers who are exposed to lead can bring it home in dust on their clothing, shoes or hair. When this dust gets into their homes, the neurotoxin can be hazardous for the whole family, but especially children, because their brains are still developing.
Ceballos has confirmed that the homes of lead-exposed construction workers can have elevated levels of lead and other metals. But preventing these exposures can be challenging because construction workers often change job sites frequently and may not have the time or resources to change clothes or shower before going home.
“Lead is the culprit we know most about” when it comes to take-home exposures, Ceballos said, “and yet there is still a lack of policy addressing the issue.”
To tackle the problem, Ceballos is using novel methods to detect lead contamination and reduce exposures at home with funding from the U.S. Department of Housing and Urban Development.
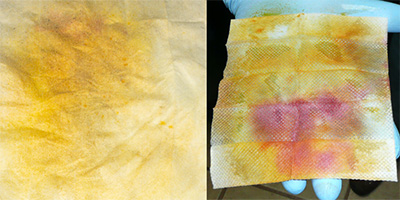
In one study, she and her team sampled the homes and cars of construction workers with colorimetric wipes that turn light orange, orange or red when there is low, medium or high potential for lead contamination on a surface, respectively.
When a wipe turned red, the workers and their families “understood there was an issue,” she said. “Even the kids got into it.” The researchers then gave families lead cleaning materials and recorded their use in the home.
Ceballos has also detected lead in the toenails of construction workers’ families using a noninvasive method called X-ray fluorescence. “It’s a much easier analysis than blood, and thus may pave the way to do easier surveillance at the community level,” she said.
Finally, she has developed new educational interventions at the community and home levels to reduce lead exposure, augmenting research focused on educating workers at their workplaces.
Ceballos and her team worked with a nonprofit organization in a pilot study to create graphic stories about the sequence of best practices for workers in any lead-exposed industry, including detailed instructions for outdoor, factory and small business workplaces.
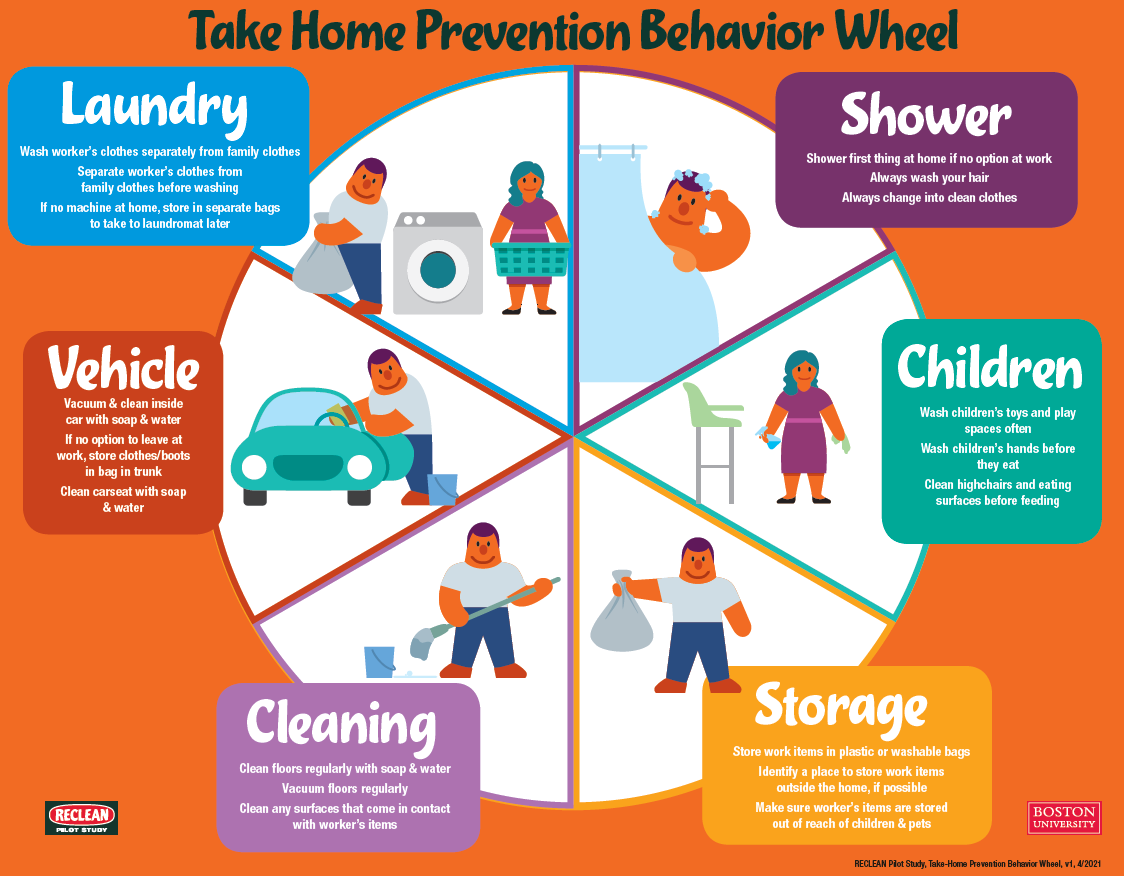
Most recently, Ceballos was inspired by intervention-based studies with farmworkers and their families done by the late Richard Fenske, formerly a DEOHS professor. Using a similar approach, she and colleagues designed educational materials highlighting a range of practical habits to prevent lead contamination for construction workers.
The materials provide one guide for workers and another for their families, with versions in English and Spanish. They are colorful and interactive: after a checklist, readers can follow five to six recommendations oriented around a wheel with categories like “clothing” and “storage.”
They also offer options for best practices in each category — such as changing clothes and boots before returning home “when you can” — and alternatives for “when you can’t,” like wearing a protective outer layer to remove before coming home. Workers and caregivers in the study used them to create action plans, including the top lead-prevention practices they felt able and motivated to address first.
The researchers carried out a pilot study of the materials with 33 construction workers and 11 of the workers’ family members. On average, participants’ test scores evaluating knowledge of take-home exposure to lead increased 11 points after reading the materials.
Notably, participants younger than 30 were more likely to have a lower initial test score, indicating the importance of educating children of workers.
Untangling exposures for children in agricultural communities
Children in agricultural communities, including the families of farmworkers, are at risk of exposure to a wide range of pollutants, including pesticides, fertilizers, dust, wildfire smoke, woodstove emissions, and gases and small particles derived from animal waste.

DEOHS Professor Catherine Karr and collaborators have shown that exposure to agricultural pollution may partially explain why children in the Lower Yakima Valley — a major farming region of Washington state — have significant rates of death from asthma despite experiencing lower levels of traffic emissions than urban kids.
Now a new research center in the department led by DEOHS Professor Elaine Faustman aims to assess the cumulative impact of these chemical stressors, as well as psychosocial stress, by tracking biomarkers related to the exposures and their health effects in study participants in the valley.
The researchers are analyzing blood and urine samples and questionnaires from a cohort previously characterized by Faustman, Fenske and others through the former UW Center for Child Environmental Health Risks Research.
Their earlier research showed that farmworkers’ children were exposed to pesticides through take-home and other pathways, and partnered with families to create effective interventions to reduce these exposures. The study cohort includes children and adults in 100 households in the valley, 60 including farmworkers and 40 households without them, with samples spanning from 2005 to 2011.

The new center, called Integrating and Informing Actionable Agricultural Community Tools (II-ACT), will examine pesticides, phthalates and metals in house and vehicle dust from study participants, and compare them with pesticide metabolites and other biomarkers linked to respiratory, neurologic and metabolic health.
These “sensitive and specific measurements can link agricultural exposures to outcomes like adverse respiratory health events, allowing us to better protect children’s health in these historically underserved agricultural communities,” said Hannah Dye, an MS student in DEOHS who is involved in the project.
In addition to biomarker work led by Faustman and DEOHS Assistant Professor Judit Marsillach, the new center will map cumulative environmental health impacts in efforts led by DEOHS Professor Edmund Seto and Clinical Assistant Professor Esther Min.
It will also build on the department’s long-term partnership with the community on this research through a translation core led by Karr and Yakima-based community liaison Elizabeth Torres.

Because the samples follow the same cohort over many years, the researchers hope to determine the impact of policy changes, such as pesticides that were regulated in the interim.
“One of the biggest things about this project is the cohort itself. It really shows the commitment of the community members to protecting their children's health,” Dye said. “Having that longitudinal follow-up allows us to answer questions about whether these regulations are curbing exposures, and assess whether they are having an effect on children's health.”
Support for healthcare workers in the pandemic and beyond
In the early months of the COVID-19 pandemic, healthcare workers in the U.S. were swamped by long and arduous hours, uncertainty about the dangers of the virus and a scarcity of adequate personal protective equipment (PPE), with vaccines still a year or more in the future.
Layered over these stressors was the concern of spreading the virus to their families or housemates, and a lack of clear protocols from their workplaces about how to avoid this.
In early 2020, Ceballos and colleagues surveyed 234 healthcare workers and interviewed a subset of 23 of them to understand how they were reacting to the situation and what could be done to improve it.

They found that workers used strategies ranging from isolating from their families entirely to disinfecting, changing clothes and using PPE such as masks in their cars and at home.
Workers also experienced significant stress and anxiety about how to prevent transmission to their households, particularly the one-third of respondents who had people vulnerable to COVID at home.
“I wouldn’t even touch my kids or say hi to my kids. I’d run upstairs and take a shower; then I would come down,” wrote one survey respondent.
Another shared: “I don’t have a locker… So, [I would] go into the staff bathroom, put a sheet on the floor, disrobe everything away from [my] body; it was all contaminated. Put on clean scrubs, put the dirty scrubs back into a bag that could be washed, and then wash my hands because we were worried that anything you touched could be spreading the virus.”
Fortunately, the hospital in the study offered many resources to workers and their families as they became available, such as COVID-19 tests and vaccines. Regardless, the researchers concluded that healthcare workplaces could learn from the COVID-19 pandemic to better protect workers and their families in future pandemics.
According to their recommendations, employers need to create consistent protocols and resources for all healthcare workers, not just those directly exposed to sick patients, to prevent the spread of disease outside of hospitals.
Most important, there is a need to strengthen controls for when workers are leaving to go home, such as providing lockers and spaces to change into clean clothes, shower, and wash clothes at work.
“I wouldn’t even touch my kids or say hi to my kids. I’d run upstairs and take a shower; then I would come down.”
- Survey respondent working in healthcare during the COVID-19 pandemic
These strategies could improve mental health and job retention among healthcare workers in addition to keeping illness from spreading, the researchers note in their paper.
Ceballos was surprised to find similar concerns among workers in such different jobs as construction and healthcare, indicating how the issue of take-home exposures intersects many different fields.
“All these interventions could be done in other industries,” she said. “I think that that’s why I’m interested, because it highlights my concerns about health equity. There are a lot of people who get forgotten.”
Resources
- Ceballos cocreated guides for leaving lead at home in English and Spanish for construction workers and their families:
- The Pacific Northwest Agricultural Safety and Health (PNASH) Center, part of DEOHS, collaborated with farmers, educators and researchers in Washington state to codevelop a guide of 24 recommendations called Practical Solutions for Pesticide Safety.
- The PNASH Center also developed online, on-demand courses on pesticide safety solutions and minimizing family exposures for agricultural communities.




